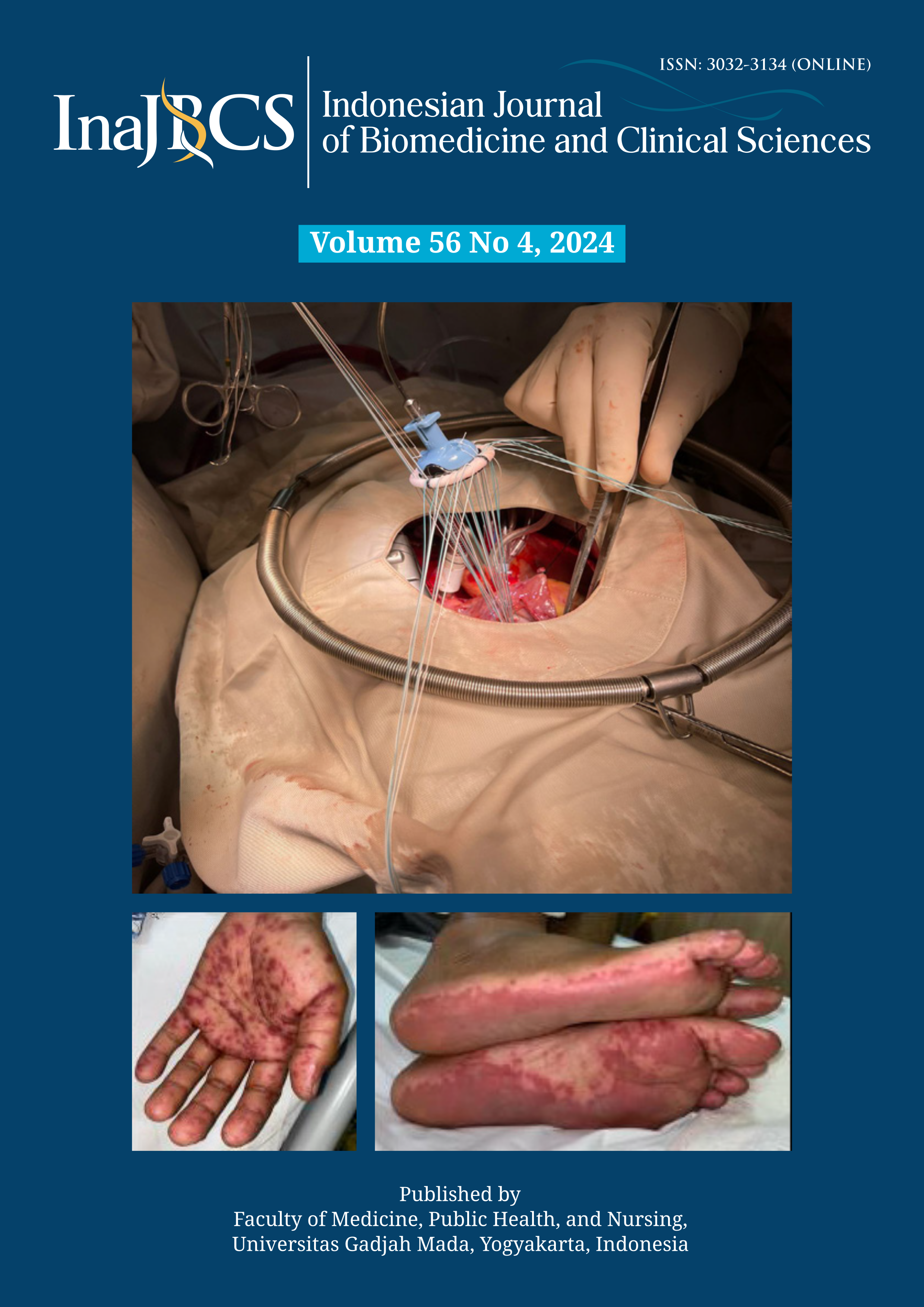
Triple valve replacement on rheumatic heart disease patient: a case report
Abstract
Triple valve replacement surgery is a complex, open-heart surgery to permanently replace all three heart valves (mitral, aorta, and tricuspid) in situations such as valvular diseases as complications of rheumatic heart disease. The expected outcome of the surgery is the proper functioning of the heart valves and the improvement of intracardiac blood flow. Triple valve replacement surgery is still considered a challenging procedure to be performed in developing countries including Indonesia due to its complexity and difficulties. The procedure needs a capable surgeon followed by the prolonged use of cardiopulmonary bypass machines and aortic cross-clamping procedures. This study presented the result of a successful triple valve replacement surgery on a 45 y.o. female with rheumatic heart disease who has manifested into cardiac valve complications. Follow-up examinations conducted directly after surgery, on the 1st, 8th postoperative day, and six months after discharge showed the desired outcome of well-functioning mechanical valves and normal global systolic function of the left ventricle, without significant postoperative cardiac events and complications. The result indicated that triple valve replacement surgery is a safe and effective procedure for rheumatic heart disease patients requiring surgical replacement of all three heart valves, encouraging more implementation of this procedure.
References
https://doi.org/10.2147/CLEP.S12977
2. Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, et al. Global, regional, and national burden of rheumatic heart disease, 1990-2015. N Engl J Med 2017; 377(8):713-22.
https://doi.org/10.1056/NEJMoa1603693
3. Lilyasari O, Prakoso R, Kurniawati Y, Roebiono PS, Rahajoe AU, Sakidjan I, et al. Clinical profile and management of rheumatic heart disease in children and young adults at a tertiary cardiac center in Indonesia. Front Surg 2020; 7:47.
https://doi.org/10.3389/fsurg.2020.00047
4. Shinn SH, Oh SS, Na CY, Lee CH, Lim HG, Kim JH, et al. Short- and Long-Term Results of triple valve surgery: a single center experience. J Korean Med Sci 2009; 24(5):818-23.
https://doi.org/10.3346/jkms.2009.24.5.818
5. Davarpasand T, Hosseinsabet A. Triple valve replacement for rheumatic heart disease: short- and mid-term survival in modern era. Interact Cardiovasc Thorac Surg 2015; 20(3):359-64.
https://doi.org/10.1093/icvts/ivu400
6. Reményi B, Wilson N, Steer A, Ferreira B, Kado J, Kumar K, et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease—an evidence-based guideline. Nat Rev Cardiol 2012; 9(5):297-309.
https://doi.org/10.1038/nrcardio.2012.7
7. Dass C, Kanmanthareddy A. Rheumatic heart disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Apr 10].
http://www.ncbi.nlm.nih.gov/books/NBK538286/
8. Sembiring YE, Ginting A, Puruhito, Budiono. Validation of EuroSCORE II to predict mortality in post-cardiac surgery patients in East Java tertiary hospital. Med J Indones 2021; 30(1):54-9.
https://doi.org/10.13181/mji.oa.204536
9. Alsoufi B, Rao V, Borger MA, Maganti M, Armstrong S, Feindel CM, et al. Short- and long-term results of triple valve surgery in the modern era. Ann Thorac Surg 2006; 81(6):2172-7; discussion 2177-8.
https://doi.org/10.1016/j.athoracsur.2006.01.072
10. Forsberg LM, Tamás É, Vánky F, Nielsen NE, Engvall J, Nylander E. Left and right ventricular function in aortic stenosis patients 8 weeks post-transcatheter aortic valve implantation or surgical aortic valve replacement. Eur J Echocardiogr 2011; 12(8):603-11.
https://doi.org/10.1093/ejechocard/jer085
11. Jasinski M, Kadzioła Z, Bachowski R, Domaradzki W, Wenzel-Jasinska I, Piekarski M, et al. Comparison of retrograde versus antegrade cold blood cardioplegia: randomized trial in elective coronary artery bypass patients. Eur J Cardiothorac Surg 1997; 12(4):620-6.
https://doi.org/10.1016/s1010-7940(97)00213-3
12. Zanobini M, Saccocci M, Tamborini G, Veglia F, Di Minno A, Poggio P, et al. Postoperative echocardiographic reduction of right ventricular function: is pericardial opening modality the main culprit? Biomed Res Int 2017; 2017:4808757.
https://doi.org/10.1155/2017/4808757
13. Lancellotti P, Pibarot P, Chambers J, Edvardsen T, Delgado V, Dulgheru R, et al. Recommendations for the imaging assessment of prosthetic heart valves: a report from the European Association of Cardiovascular Imaging endorsed by the Chinese Society of Echocardiography, the Inter-American Society of Echocardiography, and the Brazilian Department of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2016; 17(6):589-90.
https://doi.org/10.1093/ehjci/jew025
14. Gupta S, Chowdhury D, Biswas P. Triple valve replacement: a case report. JNHFB 2019; 8:42–4.
15. Leone A, Fortuna D, Gabbieri D, Nicolini F, Contini GA, Pigini F, et al. Triple valve surgery: results from a multicenter experience. J Cardiovasc Med (Hagerstown) 2018; 19(7):382-8.
https://doi.org/10.2459/JCM.0000000000000665
16. Ahmed T, Shkullaku M, Chahal D, Dawood M, Gupta A. Triple valve replacement in a patient with severe combined aortic and mitral stenosis. Cureus 202; 12(3):e7412
https://doi.org/0.7759/cureus.7412