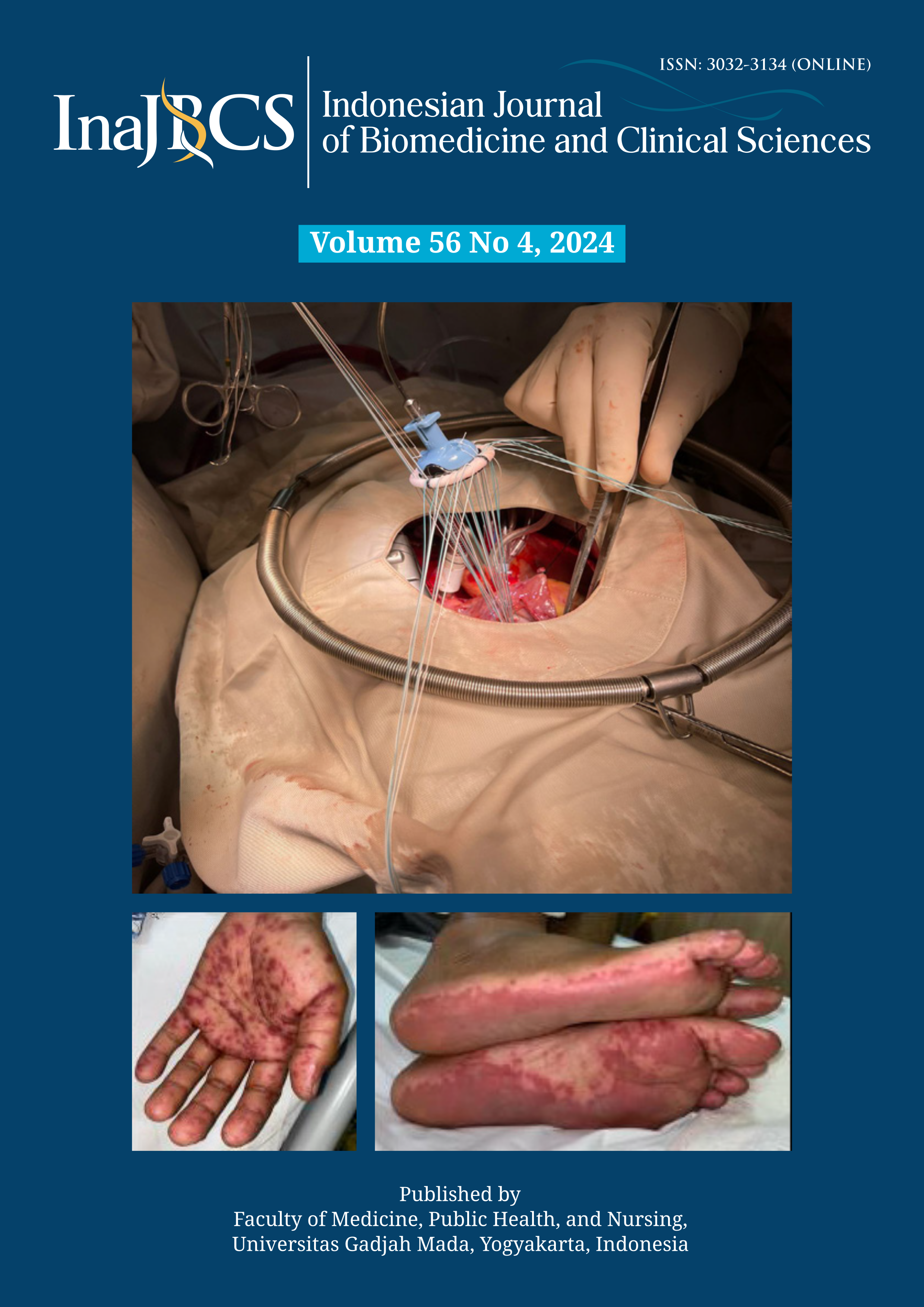
Treatment challenges of nevirapine-induced Stevens-Johnson syndrome: a case report
Abstract
Nevirapine, a non-nucleoside reverse transcriptase inhibitor (NNRTI), is a crucial component of antiretroviral therapy (ART) in HIV management. However, nevirapine carries a rare but potentially life-threatening risk of Stevens-Johnson syndrome (SJS). We reported a case of severe cutaneous manifestations of extensive necrolysis in an HIV-positive patient on the ARV nevirapine. This case highlights the importance of recognizing nevirapine-induced SJS, particularly in the early stages, to ensure prompt discontinuation of the drug and initiation of appropriate supportive care. Clinicians managing HIV patients on nevirapine-based ART should remain vigilant for early signs of SJS and maintain a high index of suspicion.
References
Arts EJ, Hazuda DJ. HIV-1 antiretroviral drug therapy. Cold Spring Harb Perspect Med 2012; 2(4):a007161.
https://doi.org/10.1101/cshperspect.a007161
Limou S, Winkler CA, Wester CW. HIV pharmacogenetics and pharmacogenomics: From bench to bedside. Genomic and Precision Medicine 2019; 185-222.
https://doi.org/10.1016/B978-0-12-801496-7.00013-7
Maharani PN, Suwarsa O, Prodjosoewojo S. Clinical profile of adverse cutaenous drug reactions in patients with human immunodeficiency virus. Althea Med J 2020; 7(4):200–5.
Wibisono Y, Agusni I, Hidayati AN, Rahmadewi, Astindari, Sari M, Murtiastutik D, et al. Cutaneous adverse drug reactions in hospitalized HIV / AIDS patients. Period Dermatol Venereol 2018; 96-102.
https://doi.org/10.20473/bikk.V33.2.2021.96-102
Kawalec P, Kryst J, Mikrut A, Pilc A. Nevirapine-based regimens in HIV-infected antiretroviral-naive patients: systematic review and meta-analysis of randomized controlled trials. PLoS One 2013; 8(10):e76587.
https://doi.org/10.1371/journal.pone.0076587
Coleman JJ, Pontefract SK. Adverse drug reactions. Clin Med (Lond) 2016; 16(5):481-5.
https://doi.org/ 10.7861/clinmedicine.16-5-481
Hoosen K, Mosam A, Dlova NC, Grayson W. An update on adverse cutaneous drug reactions in HIV/AIDS. Dermatopathology (Basel) 2019; 6(2):111-25.
https://doi.org/10.1159/000496389
Kakande B, Isaacs T, Muloiwa R, Dlamini S, Lehloenya R. Case report: Stevens-Johnson syndrome following a single double dosing of nevirapine-containing regimen once in an HIV-infected woman on long-term antiretroviral therapy. F1000Res. 2015; 4:175.
Chateau A V, Dlova NC, Dawood H, Aldous C. Outcomes of Stevens-Johnson syndrome and toxic epidermal necrolysis in HIV-infected patients when using systemic steroids and/or intravenous immunoglobulins in Pietermaritzburg, South Africa. South Afr J HIV Med 2019; 20(1):944.
https://doi.org/10.4102/sajhivmed.v20i1.944
Pawar MP, Pore SM, Pradhan SN, Burute SR, Bhoi UY, Ramanand SJ. Nevirapine: most common cause of cutaneous adverse drug reactions in an Outpatient Department of a Tertiary Care Hospital. J Clin Diagn Res 2015; 9(11):FC17-20.
https://doi.org/10.7860/JCDR/2015/13672.6768
World Health Organization. Guidelines on the treatment of skin and oral HIV-associated conditions in children and adults. National Library of Medicine. 2014.
Kouotou EA, Nansseu JR, Ngono VN, Tatah SA, Zoung-Kanyi Bissek AC, Ndjitoyap Ndam EC. Prevalence and clinical profile of drug eruptions among antiretroviral therapy-exposed HIV infected people in Yaoundé, Cameroon. Dermatol Res Pract 2017; 2017(1):6216193.
https://doi.org/10.1155/2017/6216193
Lu-Hui Yang, Jun-Ting Tang, Xi-Chuan Yang TWZ. Mucocutaneous manifestations of HIV/AIDS. Springer International Publishing 2020; 237-61.
Mohseni Afshar Z, Goodarzi A, Emadi SN, Miladi R, Shakoei S, Janbakhsh A, et al. A Comprehensive review on HIV-associated dermatologic manifestations: from epidemiology to clinical management. Int J Microbiol 2023; 2023:6203193.
https://doi.org/10.1155/2023/6203193
Tseng J, Maurer T, Mutizwa MM. HIV-associated toxic epidermal necrolysis at San Francisco General Hospital. J Int Assoc Provid AIDS Care 2017; 16(1):37-41.
https://doi.org/10.1177/2325957415614651
Sharma AM, Klarskov K, Uetrecht J. Nevirapine bioactivation and covalent binding in the skin. Chem Res Toxicol 2013; 26(3):410-21.
https://doi.org/10.1021/tx3004938
Umapathy S, Pawar A, Bajpai S, Pazare AR, Ghosh K. HLA involvement in nevirapine-induced dermatological reaction in antiretroviral-treated HIV-1 patients. J Pharmacol Pharmacother 2011; 2(2):114-5.
https://doi.org/10.4103/0976-500X.81905
Hasan M, Yunihastuti E, Abdullah M. Incidence and predictors of nevirapine and efavirenz-associated rash among Indonesian HIV patients. Asian Pac J Allergy Immunol 2020; 40(2):141-6.
https://doi.org/10.12932/AP-080719-0596
Zhang C, Wang W, Zhou M, Han Y, Xie J, Qiu Z, et al. The interaction of CD4 T-cell count and nevirapine hepatotoxicity in China: a change in national treatment guidelines may be warranted. J Acquir Immune Defic Syndr 2013; 62(5):540-5.
https://doi.org/10.1097/QAI.0b013e3182845cc7.
Pott Junior H, Gosuen GC, Gales AC. DRESS syndrome due to nevirapine treated with methylprednisolone. Case Rep Med 2013; 2013:269501.